Many of the issues caused by narcotic use and abuse are known, and most of these are physical issues, especially those associated with overdose. However, opiate-induced depression can occur in certain situations, and it can be just as dangerous or problematic as mental disorders that occur outside of drug use.
How Can Narcotics Cause Depression?

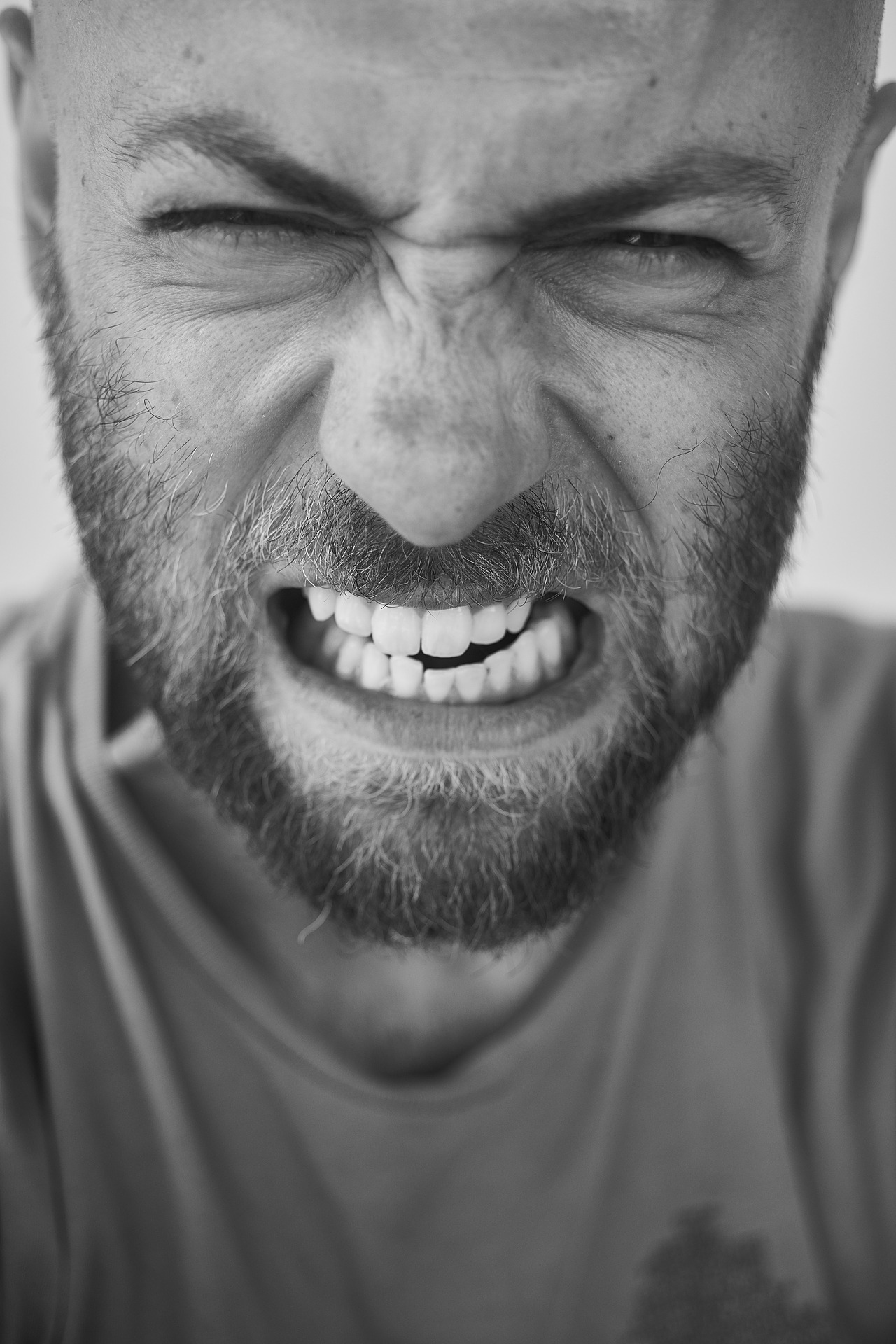
Depression is a common narcotic withdrawal symptom.
In most instances, if you take opioids as prescribed and are weaned off them safely through the care of a doctor once you are ready to stop taking them, you will not experience increased levels of depression. However, those who go through withdrawal without medical assistance (especially without the use of pharmaceuticals to minimize their symptoms) are likely to experience some depressive symptoms caused by withdrawal. This can occur whether a person has been abusing the drug or not but is more likely to happen as the result of abuse.
According to the National Library of Medicine, “Those withdrawing from opiates should be checked for depression and other mental illnesses.” This is because it is common for individuals who abuse illicit drugs heavily to also have a comorbid mental disorder, but the narcotic withdrawal syndrome itself can cause depressive symptoms that may become very intense based on the severity of the individual’s drug abuse, other psychological issues, etc.
In addition, Saint Louis University cited a recent study that found “a link between chronic use of pain-relieving medication and increase in the risk of developing major depression.” As individuals who had never had issues with the mental disorder before continue to show signs of it after taking the medication for a prolonged amount of time, “these findings suggest that the longer one is exposed to opioid analgesics, the greater is there risk of developing depression.”
Therefore, narcotic- or opiate-induced depression can occur either while an individual is taking the medication, after having taken it for a long time, or while going through withdrawal. Though abuse likely increases this risk, those who take their medication as prescribed can also develop these issues.
How Can Opiate-Induced Depression Be Treated?
It is important that we understand the issue for what it is: this is not a milder form of depression or something that will likely fade away after the individual’s dependence on opioids does. It is a serious condition that should be treated along with any drug abuse, addiction, or dependency issues the individual may be struggling with.
Those experiencing opiate-induced depression will require treatment that addresses both their drug use and their depressive symptoms, often with the use of behavioral therapy and possibly even pharmacological treatment. As stated by the NLM, “Antidepressant medications should NOT be withheld under the assumption that the depression is only related to withdrawal and not a pre-existing condition.” Both disorders should be treated together so the individual can begin to recover from them simultaneously; this minimizes the chance of relapse in either case.
Do You Have More Questions About Opiate-Induced Depression?
Call 800-934-1582(Sponsored) . We can answer any questions you may have about the disorder, as well as other issues associated with narcotic use and abuse. We can also help you find a treatment center in your area where you can begin to recover.
In many cases, narcotic tolerance occurs as a natural result of opioid drug use. Even if you are taking your medication as your doctor prescribed, it is likely that you will develop a tolerance to it over time, especially if you are on the medication for more than a few months. However, even though it is difficult to prevent, narcotic tolerance can be dangerous and should be monitored for any problematic effects.
What are the Dangers of Tolerance?

Narcotic tolerance can lead to dependence and addiction.
According to the National Institute on Drug Abuse, “Tolerance occurs when the person no longer responds to the drug in the way that person initially responded.” They will need higher doses of that drug in order to feel the same effects they felt from the lower dose previously. This is normal and should be handled by your doctor during treatment. You may be placed on a different medication altogether, but sometimes, the dosage is increased to combat the issue. This can be a dangerous path.
Many times, when the dosage is increased, it is only a temporary fix. And, according to a study from the American Association of Pharmaceutical Scientists Journal, a person’s tolerance to the side effects caused by opioids usually does not increase with their tolerance to its analgesic effects. “It is the inability to tolerate these undesirable side effects that eventually limits dose escalations and analgesic efficacy.”
Nevertheless, the individual’s tolerance for the drug’s analgesic effects will often continue to grow steadily higher if they receive increased doses, and they will need more and more of the drug each time in order to feel its effects. If your treatment is being managed by a doctor, you are likely in good hands, but some individuals begin to feel that they should be able to choose their own dosage level in order to combat this issue. This is where the serious risks caused by narcotic tolerance usually come in.
Any time you start taking your medication in a dosage other than what your doctor has prescribed, you are abusing your prescription, and opioid abuse can lead to overdose, addiction, dependence, and possibly even heroin abuse.
How Can I Avoid the Issues Associated with Narcotic Tolerance?
Talk to your doctor right away if you begin to notice that your tolerance for the drug is increasing. Discuss with them that you are concerned about the way opioid tolerance can affect you. If it is safe for you to begin withdrawing from the medication, you may decide to do so, but some individuals do need to stay on pain medication for a longer period of time. No matter what, you must discuss the issue with your doctor, and you must never attempt to increase your dosage yourself. This can be very dangerous and leads many toward addiction.
Don’t Allow Your Tolerance to Control You
Tolerance in general is not an issue. But the behavior it may create can be extremely problematic if not kept in check. Always make sure to discuss with your doctor any problems you are having with your medication, especially if you feel that you are likely to abuse the medication to get your desired effects. This can only lead to serious problems and should be avoided at all costs. If you would like to learn more about narcotics, call 800-934-1582(Sponsored) .
Codeine is a dangerous drug that, recently, has been abused most often by adolescents in the form of cough syrup. This is because it can “produce relaxation and euphoria when consumed in sufficient quantities,” but because the medication is not meant to be taken for this purpose, its use can be dangerous (National Institute on Drug Abuse). Still, how can you know if your codeine abuse has gotten out of control?
Signs of Problematic Codeine Abuse

Codeine abuse can lead to intense cravings, where you feel like you need it to get through the day.
Someone who takes codeine cough syrup––or any form of the narcotic––in high enough doses to cause euphoria even one time could potentially overdose, causing severe respiratory depression and possibly death. But if you have been abusing codeine frequently, here are some of the signs that your drug use may have gotten unmanageable.
- You think about using codeine even when you are not.
- You feel yourself becoming more and more tolerant to the drug every time you take it, and in order to counteract that tolerance, you drink or otherwise abuse more each time.
- You frequently mix codeine cough syrup with alcohol or take the tablets, capsules, etc. while drinking.
- You are abusing the drug with increased frequency, taking it more often than you used to.
- You take codeine even when you are alone.
- You notice that you have begun to crave the drug.
- When you find out you cannot take the drug, it makes you very angry, depressed, or upset.
- You have begun to obtain codeine illegally by stealing prescriptions or by doctor shopping.
- You spend money you don’t have or money that was meant for other things on codeine.
- You’ve stolen to obtain the drug.
- You’ve lied in order to use or obtain the drug.
- Your friends or family members have expressed concern about your codeine use.
- You do not feel that you could get through the day without the drug.
- You make excuses to take the drug.
- You have experienced moderate to severe side effects as a result of your frequent codeine use and yet you refuse to stop taking it.
If the statements above accurately reflect your situation, your codeine use has gotten out of control and become very dangerous. As a narcotic, this drug can cause all the same problems that other prescription opioids can, and your regular and risky use of it likely requires treatment.
Can You Become Addicted to Codeine?
Codeine is an opioid and, therefore, can become addictive. According to the NIDA for Teens, “People who abuse prescription opioids are at greater risk [for addiction] than people who take them as prescribed,” and the behaviors above are warning signs of addiction. If these statements are similar to your experience, your use of codeine has become dangerous and you must attend treatment immediately. Addiction to opioids can be very problematic, and the sooner it is treated, the better.
You can always begin your recovery, especially if you have begun to recognize the severity of your drug abuse. If you would like to find a treatment program or ask more questions about codeine abuse and its dangers, call 800-934-1582(Sponsored) .
Technically, all drugs are not considered narcotics. The current definition of the term is often confused many individuals, but only one specific class of drugs is considered to be synonymous with it: that of opioid analgesics.
Which Drugs are Narcotics?
According to the Drug Enforcement Administration, “‘Narcotic’ refers to opium, opium derivatives, and their semi-synthetic substitutes.” The term that is synonymous with narcotics is opioids. These drugs can include both prescription and illicit substances as long as they fall into the category of opioid analgesics. As stated by the National Institute on Drug Abuse, the most commonly abused narcotics include:
- Heroin
- Opium
- Codeine
- Fentanyl
- Hydrocodone
- Hydromorphone
- Meperidine
- Methadone
- Morphine
- Oxycodone
- Oxymorphone
There are many other derivatives of these specific drugs that are also opioids, but in general, if a substance is not an opioid or does not have opiate properties, it is not considered to be a narcotic. Still, many individuals use the word as a blanket term to describe all drugs or to describe only illegal or illicit drugs.
Why is Narcotic Used Differently?
According to the DEA, “The term ‘narcotic’ comes form the Greek word for ‘stupor’ and originally referred to a variety of substances that dulled the senses and relieved pain.” This term also extended to drugs and other substances that had sleep-inducing properties. Though the term has been narrowed considerably to only include opioids in the medical world, there are some differences in how it is treated in the legal world.
Often, the term is used to refer to any substance that is being used illegally, whether it is a Schedule I drug that has no legal or medical use or whether it is a prescription medication that an individual has abused in order to experience certain effects that were not intended by the prescription. For this reason, the term narcotic has a bad connotation, and when people say they are taking a drug of this type, it often sounds like they are doing something wrong.
In many places, this definition has snowballed, and all drugs have come to be referred to as narcotics. Different people might mean different things when using this term, whether they realize it or not.
Which is the Correct Usage of the Term?

Many people don’t know which drugs are actually narcotics.
For certain, all drugs are absolutely not narcotics. Even in some cases when more substances are referred to by this term, it does not cover every type of drug or psychoactive substance available for use or abuse.
Because of the connotations as well as the original Greek meaning of the term, it can be much safer to use the term narcotic only when you are referring to “opioid pain relievers” or other opioid-based drugs, as stated by the National Library of Medicine. Stimulants do not cause relaxation and stupor the way opioids do, so using the term this way makes the distinction clearer. In addition, most individuals in the medical community will use the term interchangeably with all types of opioids––legal and illegal––making this perhaps the clearest definition of the term.
Do You Want to Learn More About Narcotics?
Call 800-934-1582(Sponsored) . We can answer any questions you may have about this drug class as well as discuss the substances that fall into this category so you can learn more.
Tramadol, brand name Ultram, is used to treat pain in the same way other opioids are. While it can be a beneficial medication for some individuals, tramadol, like all opioid drugs, can cause withdrawal if a person suddenly stops taking it. However, the withdrawal syndrome associated with this medication can sometimes be even more dangerous than that caused by other opioid drugs.
Tramadol vs. Regular Opioid Withdrawal
According to the National Library of Medicine, “Opioid withdrawal reactions are very uncomfortable but are not life-threatening.” Most of the concern related to this syndrome is the high possibility for relapse based on the uncomfortable symptoms, such as muscle, bone, and joint pain and severe flu-like effects. This is why people attempting to stop using or abusing opioids are urged to attend professional care, even though the syndrome itself may not be deadly.
Tramadol, on the other hand, causes many of the same withdrawal symptoms caused by other opioids, but it can also cause other symptoms that are not seen in any other syndrome associated with these specific drugs. Regular opioid withdrawal, according to the US Department of Justice, “is encountered in about 90 percent of cases of withdrawal from tramadol.” But in about 10 percent of these cases, another syndrome is caused, leading to hallucinations, paranoia, panic attacks, severe anxiety, and “numbness and tingling in the extremities.”
Knowing this, most individuals will experience the normal symptoms caused by all opioids if they suddenly stop taking tramadol. But the possibility that they could experience these severe and sometimes-deadly symptoms can intensify the danger associated with tramadol withdrawal.
Why is the Second Type of Tramadol Withdrawal so Dangerous?

Tramadol withdrawal has the potential to cause intense anxiety.
Tramadol withdrawal can rarely cause severe psychosis in users, and this can be deadly. People do not know what they are doing when they experience hallucinations, intense anxiety, and paranoia, and these kinds of reactions can lead to confusion, aggression, and violence. Many individuals become homicidal or suicidal because they are afraid and not in control of their actions. This type of issue facing tramadol users is uncommon, but the possibility of its occurrence could make withdrawing individuals a danger to themselves or others.
How Should the Syndrome Be Treated?
While individuals going through regular opioid withdrawal should attend professional treatment to avoid the painful side effects and the possibility of relapse, those withdrawing from tramadol should attend professional treatment too. Sometimes, they will only need the same type of treatment that other opioid users require, but the syndrome may turn quickly into the more severe type, causing them to require constant monitoring and 24-hour care.
In most cases, if this more severe syndrome does occur, patients will be treated with sedative, analgesic, and hypnotic drugs but not with antipsychotics, as they would normally be if their symptoms were based on actual psychosis. According to a case report from Addiction & Health, “After 3 days all physical and mental symptoms including hallucinations and delusions completely subsided.”
Do You Want to Learn More About Tramadol?
Or do you have other questions about a narcotic use or abuse issue? Call 800-934-1582(Sponsored) today for help.
It is, unfortunately, common for prescription narcotic abusers to switch to heroin if nothing impedes their drug abuse. This is an extremely dangerous and problematic issue that can lead to further drug abuse, addiction, overdose, and death. But how likely is it for a prescription narcotic abuser to switch to heroin?
What is the Relationship Between Prescription Opioids and Heroin?
According to the National Institute on Drug Abuse, “The recent trend of a switch from prescription opioids to heroin seen in some communities in our country alerts us to the complex issues surrounding opioid addiction and the intrinsic difficulties in addressing it through any single measure such as enhanced diversion control.” Though we attempt to stop prescription opioid diversion as much as possible to help avoid the high levels of opioid abuse, the problem still occurs continuously and often. What’s more, the decreased diversion of prescription drugs that we hope to create cannot make a considerable difference if illegal heroin is still highly available.
Individuals do switch from prescription opioids to heroin for a number of reasons, not just because the second drug causes a more intense high. These reasons include:
- Heroin’s availability vs. the higher difficulty to obtain prescription opioids without a prescription
- Heroin being less expensive than prescription opioids, which are sometimes sold illegally for several dollars a pill
- The ritual of administering heroin and how some people who begin abusing prescription drugs learn to crush and snort the pills, which provides their “initiation” into this lifestyle and activity (NIDA)
- The attention currently on stopping prescription opioid abuse, which causes heroin abusers to become less of a target for law enforcement at certain times
- The fact that one person can switch back and forth between several different narcotics when one is not available and still avoid withdrawal and other issues
Because of these reasons, the switch to heroin is common––and dangerous.
How Common is It for Someone to Make the Switch?

A narcotic abuser will likely switch over to heroin at some point.
It is likely that individuals who abuse prescription opioids in large amounts and who become severely addicted and/or dependent on these drugs will switch to heroin after some time. According to the NIDA, “Nearly half of young people who inject heroin surveyed in three recent studies reported abusing prescription opioids before starting to use” the drug. These numbers are troubling, as a true pattern can be seen among narcotic abusers.
While someone who uses opioids recreationally for the first time is not likely to immediately switch to heroin, all the reasons that cause the latter drug to be more desirable to serious abusers can lead many toward heroin use. This is why it is so important that someone who is addicted, or in danger of becoming addicted, to narcotics receive treatment as soon as possible, hopefully helping them avoid the use of even more dangerous drugs.
Do You Want to Learn More about the Risks of Narcotic Abuse?
Are you looking for addiction treatment? Call 800-934-1582(Sponsored) today. We can help you with any issue you may have concerning narcotics and can answer your questions about opioid use and abuse.
There are many things you should know about withdrawal from narcotics, whether you have been abusing prescription drugs or illegal opioids or merely taking painkillers as directed by your doctor. Opioid withdrawal has many symptoms and several potential complications, and it will be much safer if you understand what is to come before the syndrome occurs.
Knowing Your Symptoms
Opioid withdrawal is uncomfortable and incredibly painful. It is important to understand this because many people do not realize how intense the symptoms will be, often leading them to attempting to quit on their own and then relapsing when they cannot handle the severity of their reaction.
Knowing the symptoms beforehand is important, and it is necessary that you consider how severe your dependency is in order to give yourself an idea of how intense they may be. Some of the common withdrawal symptoms associated with narcotics are:
- Agitation
- Muscle and joint pain
- Back pain
- Crying/tearing of the eyes
- Runny nose, sweating, chills, fever, and other flu-like symptoms
- Anxiety
- Insomnia
- Yawning
- Diarrhea
- Nausea
- Vomiting
- Abdominal cramps
- Dilated pupils
Understanding the Timeline
Depending on the drug you have been taking, opioid withdrawal can start at different times. According to the National Library of Medicine, “Symptoms usually start within 12 hours of last heroin usage and within 30 hours of last methadone exposure.” Knowing when to expect the symptoms will keep you from being caught off-guard.
Normally, the worst symptoms occur during the first one to two days of withdrawal, and many individuals experience flu-like effects at this point. This will also be the most painful time in most cases, as the back, joint, and muscle pain usually occurs during the first few days. Once it begins to subside, it will still be difficult to eat and keep anything down for several days, due to the nausea and vomiting. Still, you must drink plenty of fluids in order to avoid dehydration.
The withdrawal syndrome itself will often last for about a week, give or take a few days. According to Harvard Medical School, though, “The intensity of the reaction depends on the dose and speed of withdrawal. Short-acting opiates tend to produce more intense but briefer symptoms,” while long-acting drugs will often cause an individual to experience a longer syndrome with less intense symptoms. Still, if you experience a withdrawal syndrome that lasts more than fifteen days, something may be wrong.
Accepting Help and Treatment
Part of your research should include learning about the possible treatment options available to you and coming to understand that you should accept help during this difficult time. Treatment is often necessary for a safe, less intense withdrawal syndrome, and individuals who seek out this kind of help usually have a much less traumatic experience.
Find a rehab or detox center, doctor, or treatment option that sounds beneficial to you before you begin to go through the syndrome. We can help you look for the right withdrawal care. By calling 800-934-1582(Sponsored) , you can receive answers to any questions you may have about narcotics and withdrawal, making you more informed before you attempt to stop using these drugs and allowing your entire withdrawal experience to be safer and more tolerable.
According to the Substance Abuse and Mental Health Services Administration, “When taken as prescribed, buprenorphine is safe and effective.” The drug is well-tolerated by most of the individuals who take it, and it does not cause some of the problematic side effects caused by other treatments for opioid addiction. Though there are some issues with the drug that should be understood and considered by anyone who is considering using it, it is a safe medication that can help protect users from further drug abuse.
What Helps Make Buprenorphine Safe for Opioid Addiction Treatment?
One of the most effective parts of buprenorphine treatment, and the way in which it is able to protect users from abusing it, is that it is often given in conjunction with naloxone. The product Suboxone combines both buprenorphine and naloxone in order to protect the drug itself from abuse. Some users may attempt to crush the drug and inject or snort it, but the naloxone present in the medication will precipitate withdrawal immediately if this happens. Because buprenorphine is so regularly prescribed with naloxone, it helps protect users from relapse in this way.
According to the Journal of Neurosciences in Rural Practice, buprenorphine also has a “greatly reduced risk of overdose.” This is because the drug itself is only a partial opioid agonist, and those who take it in larger doses will be less likely to overdose than those who overuse a drug like methadone, a full agonist. The risk of respiratory depression, coma, and death are all considerably lowered during buprenorphine treatment as well, as opposed to during methadone treatment.
Compared with other pharmacological treatments for opioid addiction, buprenorphine can be safer from abuse and overdose, but like all medications, it does have side effects that can be problematic.
Are There Any Dangerous Side Effects Associated with Buprenorphine Treatment?
The main problematic side effect of buprenorphine is associated with the liver. As stated by the JNRP, “Reports already exist of buprenorphine-induced hepatitis, in particular when used intravenously.” This is because buprenorphine can elevate the liver enzymes in the individuals who take it. As a result, “national guidelines now recommend regular monitoring of liver function, especially when commencing treatment.”
However, the other side effects associated with buprenorphine are similar to those associated with other opioid-based drugs and many of the medications used to treat opioid addiction. Using illegal drugs, drinking alcohol, and taking sedatives, tranquilizers, or other drugs can be dangerous while also taking buprenorphine, as it can seriously slow one’s breathing or cause it to stop altogether. And most individuals will experience some side effects associated with the substance, but these are common ones, such as cravings, distress, irritability, nausea, and constipation.
Is Buprenorphine a Safe Treatment?
For opioid addiction, buprenorphine has been proven to be a relatively safe treatment, especially if patients take their doctor’s advice and do not deviate from their prescription amount. The drug itself can have some issues, but as long as patients are taking it as directed, it is usually very safe and effective.
If you have more questions about buprenorphine or narcotic addiction, call 800-934-1582(Sponsored) . We can help you find out about your treatment options as well as answer any other questions you may have.
Drug abuse and addiction can be devastating to the people using the drugs, as well as those around them. Unfortunately, according to the National Institute on Drug Abuse, it can be very difficult to quit, even if they want to. One of the best things you can do is to talk to someone if you would like them to get treatment. It should be noted, though, that there are right ways, and wrong ways, to talk to them about it.
Guidelines for a Successful Discussion
Saying the right thing to someone that needs drug abuse treatment is very important, if you intend to get them the help that they need. While there is no one right thing to say, there are several guidelines that you can follow to help. These include:
- expressing how much you care about them,
- setting aside a time and place for you to talk,
- discussing how their drug use is affecting them and you,
- having well-researched treatment suggestions, and
- listening to what they have to say with an open mind.
Following these guidelines makes it much more likely that your talk with them will inspire them to enter a treatment program.
What Not to Say
According to the Partnership for Drug Free Kids, there are things that you can say or do that will decrease the likelihood that the drug user you care about will seek treatment. Some of these are:
- not listening to what they have to say,
- being aggressive or confrontational,
- lecturing them instead of talking with them,
- telling them you understand, or know what they are going through (unless you have already done so yourself),
- talking to them while either of you are under the influence, and
- not having useful suggestions for treatment options.
All of these things create an environment that is not conducive to meaningful discussion of the topic of drug treatment.
Getting Them the Help They Need
The most important aspect about speaking with someone you want to seek treatment is getting them the help that they need. Addiction is a horrible and chronic disease, and it is only through treatment that recovery can be reached, and maintained. There are a number of treatment options, and there is help available for everyone that needs it. For more information on these program call us at 1- 800-934-1582(Sponsored) .
According to the National Institute on Drug Abuse, there are many things that contribute to drug addiction but there is no one predictor of it. There are however unhealthy behaviors that can contribute to the likelihood of becoming a drug addict.
Previous Addictive Behavior
Addictive behavior is a key indicator of later addiction. Although this sounds obvious, some people exhibit addictive behavior long before they ever try anything addictive. They get attached to things very quickly and have difficulty letting go when they need to.
Choosing Short Term Happiness
A very large indicator of addiction is taking short term happiness over long term goals. They take short cuts such as drinking and drugs in order to be happy. When they continue to do this it becomes a habit. Many of the substances that create short term happiness are extremely addictive. These substances include:
- opiates,
- cocaine,
- stimulants, and
- depressants such as benzodiazepines.
It also includes alcohol and many other designer drugs such as MDMA. People who desire short term happiness over long term usually end up addicted to one of these substances.
Oppositional Behavior
Defiant and oppositional behavior as a child or teenager is considered a predictor of future drug use. It is not known if it is the behavior, that is the indicator or the fact that drug use is forbidden that causes the addiction. Someone exhibiting oppositional behavior often goes against rules set by both parents and society. Using drugs is often an act of defiance unfortunately; this act of defiance can lead to addiction.
Poor Diet
Poor diet leads to a lot of health issue including depression and other mental issues. When someone is depressed or mentally unstable, they are a lot more likely to have an addiction problem than when they are not. In addition, many amphetamine addictions start with the desire to lose weight. Amphetamines are known to cause rapid weight loss and are abused because of this.
Overworking
People often use stimulants when they are overworking themselves. After awhile caffeine will no longer be enough. People who chronically overwork often turn to other stimulants. Some of those get into amphetamines. These amphetamines are extremely addictive.
Abnormal Sleeping Patterns
Abnormal sleeping patterns are both a sign and a cause of drug use. When people do not sleep, they become depressed and anxious. This causes people to start using drugs to both get themselves to sleep and keep themselves awake. Actions like this quickly cause addictions.
Isolationism
Isolationism is a cause of drug use. People suffering from social disorders and other isolationist conditions often turn to drugs for both socialization and relief. Workplace isolation can also lead to recreational drug use.
All of these unhealthy behaviors can quickly lead to drug addiction. Fortunately, there is help. If you even suspect you or someone you know is addicted to drug call us at 1- 800-934-1582(Sponsored) . We can help identify behaviors the cause addiction and help you find the treatment you need.