
Getting help for a loved one who’s struggling with addiction isn’t easy. You may be worried about their alcohol or drug use — or suffering from the consequences of their use — but you’re unsure what to do next. This is where an intervention can be helpful, but here’s the question: Do you need professional help planning an intervention?
Let’s talk about it.
What is an Intervention?
An intervention is a planned meeting where a family meets with a loved one of whom they are concerned about their drug or alcohol use. While interventions for addiction are most common, they can also be used for gambling addiction and eating disorders.
 Interventions can be held by facilitators or by family members, but it is usually recommended — given the emotional bonds you have with the family member — to seek professional help planning an intervention in this instance. Those professionals can include a social worker, doctor, therapist, or interventionist.
Interventions can be held by facilitators or by family members, but it is usually recommended — given the emotional bonds you have with the family member — to seek professional help planning an intervention in this instance. Those professionals can include a social worker, doctor, therapist, or interventionist.
Interventionists’ sole role is to facilitate a family discussion where everyone can share their concerns, provide potential solutions, and set boundaries should the person decide not to get help. They may also offer transportation to a facility after a successful intervention.
An intervention has a prescribed format, which starts before the actual meeting, and includes:
- Asking a professional for help with planning an intervention.
- Selecting a team of family members and loved ones who are concerned and can attend the intervention.
- Making a plan and setting a date.
- Conducting research about addiction and gathering information about the loved ones use pattern, the consequences, and how it has impacted the family.
- Writing statements to present to your loved one at the intervention.
- Discussing your boundaries with the intervention members should your loved one decide to reject treatment.
- Hosting a mock intervention to practice.
- Make a plan to follow up if your loved one rejects treatment and how you will support them.
In deciding whether you need professional help in planning an intervention, it’s important to consider a number of factors, including the type of substance your loved one is using harmfully. Each substance presents different risks.
Do I Need Help Planning for an Alcohol Intervention?
Alcohol addiction, also known as alcohol use disorder, can present a number of health risks from cardiovascular disease, cancer, and stroke in addition to the consequences of addictive use. According to the Centers for Disease Control and Prevention (CDC), 14.1 million Americans have alcohol use disorder. It’s a serious condition, killing 95,000 Americans every year.
While finding recovery is a positive step, stopping drinking carries risk factors for people with alcohol use disorder. It can be dangerous to suddenly stop drinking if the person is dependent. That means, if they stop abruptly, they will experience withdrawal symptoms that can include seizure and even death. So, it may be best to seek professional help.
An interventionist can help you fully prepare for the success of an intervention and support you in doing all of the intervention pre-work. This includes finding a detox facility as your loved one will likely need medical supervision and possibly medication to detox safely. You may also be asked to research a residential treatment facility that can give your loved one the best chance of sustaining their recovery.
Do I Need Help Planning for an Opioid Intervention?
 Opioid addiction, or opioid use disorder, can involve addiction to any kind of opioid, including prescription painkillers, heroin, and fentanyl. Each of these drugs are powerful – particularly fentanyl, which is a synthetic opioid that’s 100 times stronger than morphine. Opioids also carry the very real risk of fatal overdose.
Opioid addiction, or opioid use disorder, can involve addiction to any kind of opioid, including prescription painkillers, heroin, and fentanyl. Each of these drugs are powerful – particularly fentanyl, which is a synthetic opioid that’s 100 times stronger than morphine. Opioids also carry the very real risk of fatal overdose.
According to CDC data, synthetic opioids (like fentanyl) are the primary drivers of overdose deaths in the United States. During 2020 and 2021, deaths due to opioids rose 38.1 percent. It takes just two milligrams of fentanyl to cause an overdose.
Given the seriousness of opioid addiction and its risks, it may be more effective to have a professional facilitate an intervention. Here’s why.
An interventionist:
- Knows the dangers of opioids
- Understands the risks and characteristics of opioid addiction
- Is equipped to help overcome rejection
- Will keep the family on track with the intervention and toward a successful outcome
- Can provide a neutral voice and can rephrase the concerns of family members
- Are able to facilitate helpful discussion rather than blaming and punishing the person who is suffering
- Can provide transportation to a facility
Setting Up and Planning an Intervention
When in doubt, it’s perhaps best to speak to a professional who has expertise in addressing addiction and facilitating interventions.
Get help today. Call
800-934-1582(Who Answers?)
to learn about treatment programs for drug and alcohol addiction.

Setting up an intervention for a loved one is no easy task. You may be incredibly worried about their well-being and coming from a place of love, while also questioning if you’re making the right choice. You may also be asking yourself if an intervention might push them away from seeking treatment and deeper into their addiction.
These are all valid concerns. It’s important to consider the situation individually and weigh a number of factors before setting up an intervention to ensure your loved one is successful in overcoming their battle with addiction.
What is an Intervention?
An intervention is a planned process whereby an addiction professional — interventionist, doctor, or addictions counsellor — facilitates a discussion between a person struggling with substances and their concerned family members.
 The objective of the discussion is to raise concerns and confront the loved one about the effects of their substance use.
The objective of the discussion is to raise concerns and confront the loved one about the effects of their substance use.
Oftentimes an intervention is held by an intervention specialist who may draw on facilitation methods such as ARISE, SMART, or Johnson Model.
Whatever the method, the common steps involved in setting up an intervention include:
- Providing specific examples of how your loved one’s using is destructive and the effects it is having on them and the family
- Outlining boundaries that family members may set if the loved one refuses treatment
- A clearly defined treatment plan, such as a treatment center they can go to and who can accompany them there.
Things to Consider Before Setting Up an Intervention
To ensure the success of any intervention, it’s important to consider a number of factors before setting one up, including:
- Check your intentions: Ensure the motivation of the intervention is centered around supporting an individual struggling with an addictive behavior, not the opportunity to list the ways they have created harm. It is a loving and solution-oriented process not one that emotionally bashes or abuses the loved one.
- Do your research: Before setting up an intervention, you need to be knowledgeable about substance use and the factors that may indicate your loved one has a problem. An intervention may be necessary if your loved one (and possibly the family) is experiencing negative effects of their substance use; remains unable to control their use, they are in denial of the negative effects of substance use, or if their use is having a negative impact on day-to-day life.
 Use a professional: Hosting an intervention can be overwhelming. There is a lot to organize and it is often a highly emotive situation. That’s why it’s often a smart decision to use a professional during an intervention, as they can guide you through the process, act as a neutral party, and keep all members focused on the goal of supporting the loved one. The other benefits of using a professional is that they’re not emotionally involved with the person struggling or under any kind of coercion to do what the family wants. They are simply there to facilitate the discussion toward a resolution.
Use a professional: Hosting an intervention can be overwhelming. There is a lot to organize and it is often a highly emotive situation. That’s why it’s often a smart decision to use a professional during an intervention, as they can guide you through the process, act as a neutral party, and keep all members focused on the goal of supporting the loved one. The other benefits of using a professional is that they’re not emotionally involved with the person struggling or under any kind of coercion to do what the family wants. They are simply there to facilitate the discussion toward a resolution.- Plan ahead: Never set up an intervention at the last minute. Take your time to plan the intervention and collect/arrange all of the people and material that the interventionist might think will support this process. You’ll also need to think about who is going to speak, when each person will arrive, where you’ll hold the intervention, what steps you’ll take if your loved one agrees to treatment, and what you’ll do if they don’t. This can take several weeks.
- Share information: Once you have planned the intervention and selected family members to attend, share your concerns with each other and any other relevant information. This ensures that you’re a cohesive front when confronting your loved one.
- Assign roles: When sharing information, this might be an opportunity to assign tasks to each family member. For example, tasks like: researching treatment centers and calling them to see where there is availability and if they take your loved ones insurance; figuring out childcare arrangements for the loved one’s children; and speaking to your loved one’s employer (anonymously) to find out their policy for an employee needing to attend treatment.
- Anticipate their objections: It is highly likely that your loved one may object to the intervention and the idea that they should go to treatment. Remember, denial is a common feature of addiction. This isn’t an opportunity to blame or ridicule, instead think of potential objections and have solid reasons to counter them. For example, your loved one might say: “But I only drink on weekends,” to which you could contend: “Yes, but this impacts your work the next day and you’ve had X days off this year, meaning you could lose your job. You’re also failing to help out with childcare when you promised you would, which means I’ve been late to work after taking the kids to school. The effect of this is a strain on our marriage and my employer’s patience. To make up for my tardiness, I often have to work late, putting me home even later.”
If you or someone you love is experiencing a substance use disorder, help is available. Call 800-934-1582(Who Answers?) today.

I used to dread making the 100-mile drive to visit my family for Thanksgiving. I loved the food, but I was always triggered by the company.
The anxiety would kick in at least a week before – sometimes two depending on how professionally overwhelmed I was at the time – so I’d head to the store to purchase an ample selection of my favorite red wines in preparation for the four-day weekend festivities.
I loved any reason to buy more so I could save 30 percent off, nevermind the fact that I ended up consuming every bottle well in advance of the holiday.
Making Excuses for Holiday Relapse Triggers
“It’s not like I’m buying handles of vodka,” I’d unconvincingly reassure myself as I added six more mix-and-match bottles to my shopping cart the Wednesday before Thanksgiving. Deep down, my unhealed inner child was on the verge of a full blown meltdown. She knew what was coming.
At the time, the only way I knew how to help her was to sedate her with excess amounts of alcohol. Of course, I now realize that method only ended up causing more problems in the long run.
Overt boundary-pushing. Passive aggressive nitpicking. Intentional gaslighting. Unreasonable sympathy-seeking guilt trips.
At the time, the only way I knew how to help her was to sedate her with excess amounts of alcohol. Of course, I now realize that method only ended up causing more problems in the long run.
It took getting sober to realize what my triggers were, and it came as no surprise that spending extended periods of time in the company of judgmental family members with their own unresolved trauma triggered many of my anxieties that dated back to childhood.
4 Tips to Effectively Manage Holiday Relapse Triggers
 Getting sober changed my life in myriad ways. But it took a lot of hard work to get here.
Getting sober changed my life in myriad ways. But it took a lot of hard work to get here.
If you’re anything like me, you know all too well that holiday celebrations (and holiday relapse triggers) can be a slippery slope.
Whether you’re new to sobriety or COVID threw a wrench in your long-term recovery, here are four of my favorite go-to methods for staying healthy, sane, and sober this Thanksgiving.
#1 Establish a consistent, healthy routine.
I cannot stress this enough: prioritizing your well-being is not selfish, it’s an absolute necessity. If you don’t have a regular self- practice in place, set one now.
I get up at 6:30 every morning so I can have an hour of alone time to meditate, journal, stretch, and eat a nourishing breakfast. Whether I’m at home or traveling, this is my routine. No ifs, ands, or buts.
There’s no problem treating yourself (big fan of pumpkin pie, I hear you), but if all you’re doing is gorging on junk food and not making it a priority to get up and move your body, you’re on the fast track to failure.
Self-care is especially crucial when it comes to the holidays. So, make a commitment to yourself. If you don’t have an hour, 10 to 15 minutes is all you need. Remember, it’s all about consistency.
#2 Stay grounded in the present.
Feeling anxious about the thought of heading back to where it all began? Headed for a downward spiral thinking about ghosts from holidays past? Get grounded.
A daily meditation practice has been paramount to my success. Another way to quickly cultivate mindful awareness of the present moment is the 54321 technique (learn more here.) And if you like to journal or write, an activity I highly recommend for anyone who is newly soberis to spend 5-10 minutes writing a daily gratitude list.
Keep it simple. If you’re grateful for the smoothie you had for breakfast, write that down. If you struggle with the idea of putting pen to paper, verbalize it; list five things you’re grateful for when you’re brushing your teeth every morning or at night before you go to sleep.
#3 Speak kindly to yourself.
Since getting sober, I’ve done a lot of deep inner child work. I’d argue it’s one of the most powerful tools for addiction recovery because it allows you to become your own parent by consciously working with the trauma, abandonment, neglect, and/or abuse you experienced as a child.
One of the key aspects of inner child healing is the reinforcement of positive self-talk. I’m a big proponent of daily affirmations combined with EFT tapping, a form of self-help therapy that assists in reprogramming old thought patterns and beliefs.
If stress levels are high, I recommend taking at least 10-15 minutes out of your day to speak to both your present self and your inner child in a kind, loving, non-judgmental way.
Here are some powerful affirmations to get you started:
- You are safe, secure, and protected.
- You deserve to feel joy and happiness.
- You are worthy of love, respect, and support.
- I love you. I care about you. I accept you as you are.
#4 Know your boundaries…and don’t be afraid to say “no.”
 If there’s one thing I’ve learned from getting sober, it’s this: I don’t owe anyone an explanation for the way I live my life.
If there’s one thing I’ve learned from getting sober, it’s this: I don’t owe anyone an explanation for the way I live my life.
And neither do you.
If you need to limit the amount of time you spend with loved ones, set boundaries and stick to your guns. Likewise, if you feel like spending even five minutes around toxic family members this holiday season could send you over the edge, don’t do it. It’s as simple as that. Sometimes the smartest thing you can do to protect yourself is to say “no.”
Remember, it’s not selfish to put your needs first. After all, sobriety itself is an act of self-compassion. Don’t let others fool you into thinking otherwise.
For information about treatment options for you or a loved one, call 800-934-1582(Who Answers?) today.
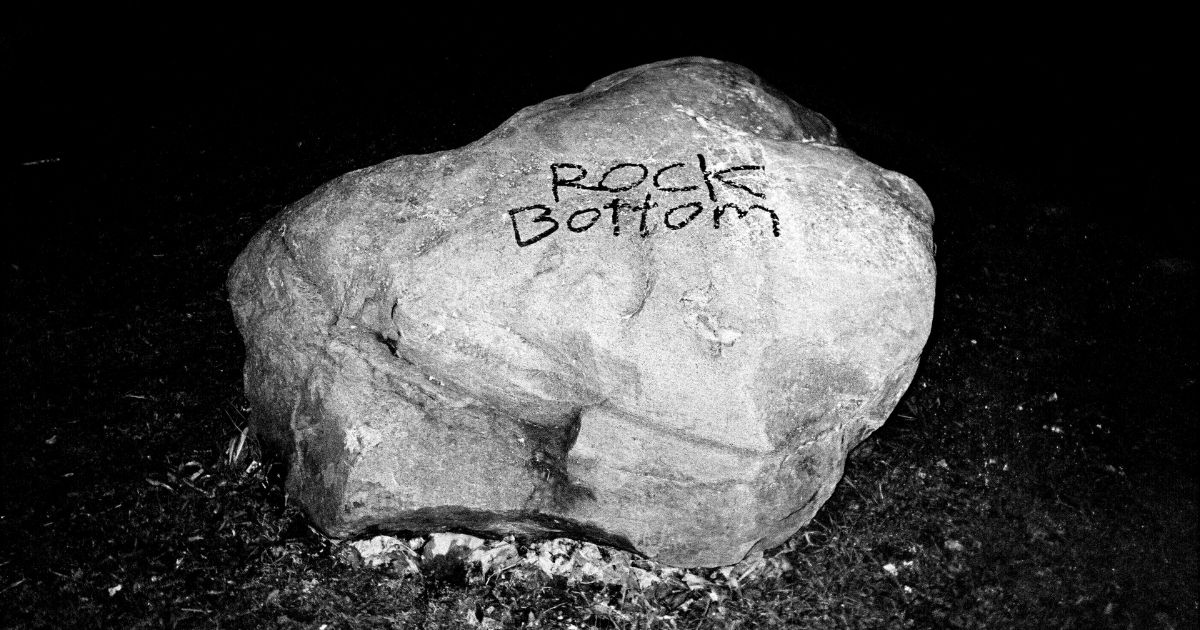
Waiting on a loved one to hit “rock bottom” before getting help for an addiction is not only harmful, it is potentially lethal. While we may have been encouraged to proceed with tough love by not “enabling” a loved one, we can inadvertently push them further into their addiction.
Instead, a more helpful approach would be to ignore the harmful rhetoric and intervene at a much earlier stage – like the grey area. It gives your loved one better chances of staying alive, and it can also prevent them from doing so much damage in the process.
Don’t Wait for Rock Bottom
I have been to countless AA meetings where the pervasive “rock bottom” myth is repeated over-and-over. The belief of many in the 12-step community is that you have to reach the depths of addiction before you can finally surrender to the disease and get help.
“He needs to go out and do more research,” Malcolm explained to me in a meeting in response to a newcomer who had relapsed. I couldn’t quite believe that a member of AA, whose only requirement of membership is a desire to stop drinking, was encouraging someone to go back to drinking until they had truly had enough.
But I experienced this more times than I wish to recall.
The reality is that not everyone reaches a rock bottom. Some people die before they reach rock bottom. Others find themselves facing a host of dangerous and life-threatening situations, such as:
- Overdose
- Buying substances laced with fentanyl
- Using alone
- Experiencing homelessness because a misguided parent kicked them out
- Not carrying naloxone because a loved one believes it enables drug use
People with substance use disorders really don’t need to be pushed to those depths. Instead, we could reach them much earlier at the gray area.
What is Gray Area Drinking?
Alcohol use disorder exists on a spectrum: from the gray area (less severe) to the more acute stages (rock bottom). About 90 percent of people who drink problematically do not have severe AUD, according to the Centers for Disease Control and Prevention.
Gray Area Drinking expert, Jolene Park explains:
“We’re all familiar with the rock-bottom kind of drinking that ruins too many lives. On the other end of the spectrum, there are those who rarely drink. If you fall in between those two extremes you might identify as a gray area drinker.”
Key signs of gray area drinking, as highlighted by Park, can include:
- Intending to have one glass of wine but finishing a bottle
- Stopping drinking for periods of time but returning because you think you have control
- Thinking and rationalizing your drinking
- Allowing drinking to prevent you from achieving the life you want
Intervening in the Gray Area
Reflecting on my own drinking, I wish I’d had an intervention at an earlier stage. I drank problematically from the time I was 13 years old.
To the outside world, I appeared to have it all: a bachelor’s degree, a place to live in the city, and a good job. On the outside, I had made it. But internally, I was progressively crumbling, over two decades.
I went from drinking a bottle of wine after work (stopping occasionally) to losing all control. I was drinking around four bottles of wine a day toward the end of my addiction. If I’d had an earlier intervention where I knew that I didn’t have to sit in a church basement and listen to sad stories, I might have gotten help much sooner.
I know that is easier said than done. As a family member, you may be afraid to confront the person dependent on alcohol or drugs. Or you may have trusted the familiar sayings in the rooms of Alanon where a family member reaches a magical “rock bottom” and instantly asks for help.
Don’t Put the Intervention Off
The reality is that If loved ones wait too long, it may actually be too late. Here are some ways you can support your loved one by intervening long before that rock bottom moment manifests:
- Model alcohol free social events: suggest to your loved one that you go for a coffee date instead of hitting a bar.
- Ask if you can cook them dinner as you’d like to discuss something on your mind. Don’t confront them, but ask them if there is anything they’re struggling with and if you can better support them.
- Tell them that you are concerned about their drinking, but not in a confrontational way. Perhaps you could say that you have noticed they’re drinking more than usual and you wondered if everything is OK. Practice active listening rather than trying to solve their problems. Ask them what their options are and if there is anything you can do.
- Be prepared by educating yourself about AUD and the options available. Ensure you have these resources to hand:
- Guidelines on normal drinking limits.
- Look for gray area digital recovery options, like Tempest, Jolene Park’s Gray Area Coaching, This Naked Mind, Workit Health.
At the end of the day, you have to decide if you’d rather overcome the anxiety of approaching the subject or deal with the shame and regret of a loved one losing his or her life to addiction. Don’t delay; intervene today.
If you or someone you love is experiencing a substance use disorder, help is available. Call 800-934-1582(Who Answers?) today.

Awareness is up. New remedies are in the works. But the stats related to the opioid epidemic are still staggering.
- Opioids were involved in nearly 50,000 overdose deaths in 2019.
- In 2019, 7 million people misused prescription pain relievers.
- In 2020, U.S. doctors wrote more than 142 million opioid prescriptions. (In some counties, they wrote enough prescriptions for every single person to have one.)
It’s a vicious cycle. Opioids are overprescribed. People take them for chronic pain. They build a tolerance. And far too many ultimately end up addicted to the drugs.
Stop the Cycle of Opioid Addiction
How does this cycle end? Perhaps by finding new remedies for pain management. Remedies that aren’t addictive.
That’s exactly what researchers like Olivier Civelli hope to do.
Civelli is a professor of pharmaceutical sciences at the UCI School of Pharmacy and Pharmaceutical Sciences and is heading up research on the use of Corydalis yanhusuo.
Is Corydalis Yanhuso an Effective Medicine to Fight Opioid Addiction?
Corydalis yanhusuo is a traditional Chinese herbal medicine. The extract of this plant, YHS, has long been used in Asian countries for the treatment of various conditions, including pain.
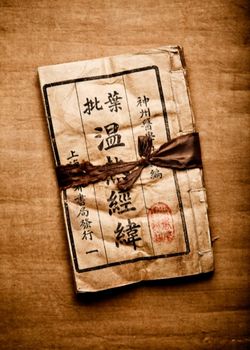 Western researchers are now looking to this herbal remedy for a potential solution to the opioid epidemic. And the results of their studies are promising.
Western researchers are now looking to this herbal remedy for a potential solution to the opioid epidemic. And the results of their studies are promising.
- It Relieves Pain
Researchers looked at the compound’s effectiveness at alleviating pain and found the herbal medicine to be effective. Because it appears to be nonaddictive, this could be a game changer for pain management. If doctors can prescribe a remedy that is both effective and nonaddictive, we could see a reduction in opioid prescriptions that may turn the tide on the opioid epidemic.
- It Reduces Addiction
Research also shows that the extract may prove helpful in reducing or preventing addiction. Civelli’s study looked at the addictive properties of morphine in mice. The research revealed that the plant extract can help curb these addictive properties. It blocks the development of morphine tolerance and dependence. Because morphine is an opioid, this suggests it would have similar results for other drugs in the opioid family, whether synthetic or natural. It might be possible to combine this extract with methadone treatments to make them more effective, or to provide the extract to patients who are on extended opioid treatments for pain. The results? The extract may help reverse current dependence and prevent future tolerance build-up that leads to new addictions.
Creating a Tool to Prevent Addiction and Overdoses
Civelli is hopeful that this research will lead to the creation of a tool that prevents addiction and overdoses. Of course, there is a long road ahead. His study was conducted on mice, and the extract will need to be tested in human trials to confirm it effectiveness. Civelli’s goal was to get the ball rolling. He wanted to establish a concept and produce results that would compel others to take the research further, to human trials.
Researchers note that the extract is currently readily available and has proven to be safe in other uses. This could help speed along the process and development of clinical trials.
Next Steps
Further research is needed. For Civelli, the next step is to look into the compound in more depth. What is it about the extract that makes it helpful to prevent addiction? How exactly does it prevent drug tolerance?
And, more research is necessary to learn more about opioids. “Why is it when people take an opioid that they need to take more and more to feel the effects?” Civelli asks.
If we can discover what is going on with the interaction between these drugs and the body, we can unlock the answer to a better way to treat pain. And that could be the secret to ending the opioid epidemic.
If you or someone you love is experiencing a substance use disorder, help is available. Call 800-934-1582(Who Answers?) today.

“When will things ever get easier,” Samantha wondered aloud. Thanks to this pandemic, she couldn’t interact with anyone for four more weeks! That’s an eternity. Samantha knows if she doesn’t have support for a single day, it feels like she’s on the verge of kissing her six weeks of sobriety goodbye. “Guess it’s time to see what these virtual NA meetings are all about.”
Whether it’s due to quarantine, car trouble, or childcare issues, many people find it hard to attend in-person Narcotics Anonymous (NA) meetings – but they need them.
For all the downsides of the Covid-19 pandemic, one bright spot has been the upsurge in online resources. Now, it’s pretty darn simple to attend an NA meeting without even leaving your house. And just like in-person meetings, these virtual meetings offer crucial support and encouragement to stay clean and sober.
How Virtual Support Groups Work
Here’s a look at how these online 12-Step meetings offer help:
- Learn how to cope: Get insights from others who have been where you are. There ARE healthy ways to deal with your emotions and stress. But they aren’t always intuitive. You have to learn the best strategies to use. Learn about them by attending a virtual meeting.
- Fight urges: How can you deal with triggers? What’s the best way to fight urges when they hit you out of nowhere? Virtual NA meetings can help you learn how to deal with these challenges. You’ll learn new insights and pick up new skills that will help you overcome even the strongest urges.
- Stay motivated: We all need encouragement. And we could use fresh ideas to stay motivated. With virtual NA meetings, you can learn new ways to keep yourself on the right track and receive encouragement from others to help you stay there. It’s good to have cheerleaders in your corner, and virtual NA meetings can help you find this support, no matter where you are physically.
- Get plugged in: You don’t have to do this alone. And you shouldn’t try to. Virtual NA meetings give you access to a strong recovery network. They plug you into resources and support that will help you maintain sobriety and allow you to thrive in the clean-and-sober life. Virtual meetings remove many challenges and barriers so you can reach out and get the help you need.
The Convenience of Virtual 12-Step Meetings
And what may be the biggest help of all? You can get all the support you need from anywhere in the world – as long as you have an Internet connection.
Virtual NA meetings offer all the above benefits of in-person meetings, but offer additional advantages.
- They work with tight schedules: No drive-time needed. Plug into a virtual NA meeting between other responsibilities of work and home. And with meetings across the nation, it’s easy to find one at all different times of day.
- They don’t require transportation: Don’t have a car? Unable to drive? Don’t want to get out during bad weather? No problem. Attend a virtual NA meeting from home.
- They don’t require childcare: Access support without finding a babysitter. You can be at home with your kids and get the help you need, with virtual NA meetings.
- They don’t require masks: Virtual meetings are perfect for those who need to follow COVID-related restrictions. Remain a safe distance while connecting when you need support most.
- They are available everywhere: Whether you’re traveling or are living in a rural area with limited in-person options, virtual NA meetings are a great way to get support anywhere in the world. Simply plug in on your favorite device and find a meeting to attend online.
Find a Virtual NA Meeting Near You
Not a tech guru? No worries. All you need is a phone, computer, or tablet to access a virtual NA meeting. Most virtual NA meetings use Zoom, Skype, or other simple video-based programs to run the meetings. These systems are easy to install on your device, and they walk you through everything step by step – so you can access virtual NA meetings in no time.
Plus, Narcotics Anonymous has a helpful directory and an easy-to-use app to help you find and attend a virtual meeting. (Android users get the app here.) You can even start your own virtual NA meeting. Here’s the scoop on how to go about doing that.
The organization has also set up a help page to provide more virtual meeting resources. With these convenient online options, it’s never been easier to get the support you need.
For information about treatment options for you or a loved one, call 800-934-1582(Who Answers?) today.
Images Courtesy of Pixabay

From trained therapy dogs to spoiled lap dogs, there’s no doubt our canine pals are amazing. And without the strength and love of my dog, I never could have overcome opioid addiction.
Some dogs play vital roles in assisted therapies, while others are tasked with jobs like searching for drugs, tracking the scent of a missing person, or alerting parents of a child’s oncoming seizure. More often than not, however, dogs serve as (wo)man’s best friend – loving us unconditionally and without an ounce of reservation.
I owe my life – and my sobriety – to Barley, a now 15-year-old Beagle/Schnauzer mix who renewed my belief in love, loyalty, and our possibilities. One look at his fuzzy little face and I melt.
Inseparable Friends
Like most wonderful things in life, I found Barley by chance. It was literally a case of being in the right place at the right time. I was minding my own business when this scruffy little 5-week-old puppy came bounding up to me…and I instantly fell in love.
 I went door-to-door in search of anyone who might know his owner. When I finally tracked this person down, the poor living conditions shocked me. I clearly remember thinking, “No wonder Barley ran away from this place.”
I went door-to-door in search of anyone who might know his owner. When I finally tracked this person down, the poor living conditions shocked me. I clearly remember thinking, “No wonder Barley ran away from this place.”
I could feel tears welling up in my eyes and a quickly growing sense of anger stirring in my spirit. “I don’t care what it takes, there’s no way I’m leaving him here. I’m going to rescue this dog,” I said to myself.
In chatting with the “owner,” it was clear she didn’t care about this precious pup. She said I could “have the damn mutt” if I wanted him. Before she could get out another word, I scooped Barley up, quickly walked away, and never looked back.
Once we got in my car, Barley jumped over the console and into my lap. I looked down and told him, “We’re going home, okay?” He immediately turned his head to the side, stood up on his hind legs, and laid his face on my neck. He knew he was safe. He knew he’d been rescued.
I grew up around dogs my whole life, but Barley was special. He’s the first dog I owned as an adult and, since I lived on my own, I could keep him inside. This sweet rescue dog won my heart, and I never went anywhere without him. We were absolutely inseparable…at least until drugs took over my life.
Loving (and Neglecting) My Best Friend
Like many other people, I started taking prescription opioid painkillers to treat a legitimate injury. In just a few short months, I developed a severe dependency on Vicodin. I was in over my head and, deep down inside, I knew it.
When you’re addicted to opioids, the bulk of your time is spent feeding that addiction. Every day, without fail, my only goal was to avoid withdrawal symptoms. I neglected my family, my friends, my job, my health – and my dog.
I often left Barley with my brother for two and three days at a time. Before I started abusing opioids, I would have been beside myself if I hadn’t seen my best buddy for a whole day, much less two or three. When I wasn’t dropping Barley off with family members, I was sleeping, working, or out looking for more pills.
I’d drive around with my poor dog in the passenger seat, riding shotgun while I was on a mission to find more drugs. And on these Vicodin-fueled trips, Barley would sit to my right, his head proudly stuck out the window, ears flapping in the wind, and nose working overtime to process scents in the air. He was so happy and content to be with me. But I was too sick to see it and too lost in addiction to care.
What an absolute waste of precious time.
Breaking My Opioid Addiction
My addiction to opioid painkillers spanned the better part of two years. And then one day, quite out of the blue, I decided it was time to get sober. I found an outpatient addiction treatment program that offered the specific therapies I needed, called them up, and made my first appointment. It’s the best decision I ever made for myself.
 I took my recovery seriously and gave it everything I had to give. I understood that, if I didn’t break the shackles of my addiction, I’d never make it out alive. I honestly couldn’t bear the thought of relapsing.
I took my recovery seriously and gave it everything I had to give. I understood that, if I didn’t break the shackles of my addiction, I’d never make it out alive. I honestly couldn’t bear the thought of relapsing.
After a few months went by, my body was rid of the drugs and the withdrawal sickness. Physically I felt wonderful; mentally I was a mess. I just felt so lost and incredibly unsure of my place in the world.
No matter where I went, I was sure that everyone saw me and knew my dirty little secret. I was an addict in recovery, and I was scared out of my mind.
Why would anyone want to be my friend? How could I ever make up for all the pain I caused? Who would ever want to love someone like me?
And then the answer licked me in the face.
My dog, my Barley, never ever left my side. My precious dog loved me no matter what kind of disease I was fighting. Every day that I didn’t have the self-esteem or courage to show my face to the world, Barley could sense it. And he would bounce around, pawing and prodding me to take him outside. He’d take his wet nose and push me, quite literally, out of the bed.
Looking in his eyes, I knew exactly what he was trying to say:
“Look mom, I love you. I’m here for you. Now get your butt up, stop feeling sorry for yourself, and let’s go live this day to the fullest.”
Embracing Life After Opioid Addiction
Believe it or not, after a few weeks of simply walking my dog and being present in the moment, my whole demeanor changed. And the miracle is that, once I began to go outside, soak up the sunshine, and breathe in the fresh air, I wanted more out of life – more out of myself.
It no longer satisfied me to hide in the house and punish myself for the mistakes of my past. I still had the support of family and real friends. I stopped worrying about things that didn’t matter. I let go of the fear and chose to embrace every day.
For too many years, I walked around believing I rescued Barley. The truth is he rescued me as much as I rescued him.
I am alive and sober today, and I owe it all to my best friend. My Barley.
Images courtesy of Pixabay and Nikki Seay
